Key points about inflammatory bowel disease
- the 2 main types of inflammatory bowel disease are Crohn's disease and ulcerative colitis
- more young tamariki are now developing inflammatory bowel disease
What is inflammatory bowel disease?
Inflammatory bowel disease (IBD) causes inflammation in the digestive system (gastrointestinal tract).
IBD is a long-lasting (chronic) condition. With effective treatment, many tamariki with IBD can remain symptom-free for long periods.
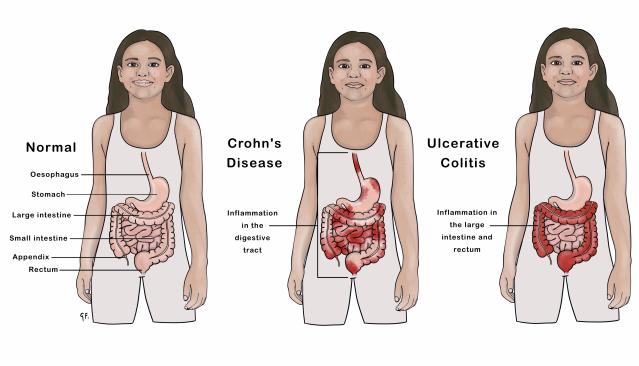
There are 2 main types of IBD. See the above illustration for the difference between a normal digestive system and one with Crohn's or ulcerative colitis.
Crohn's disease
Crohn's disease can affect any part of the digestive system from the mouth to the bottom (anus).
Ulcerative colitis
Ulcerative colitis affects the colon and rectum. The colon is also called the large bowel or large intestine.
How common is inflammatory bowel disease?
IBD has become increasingly common around the world and in particular, Crohn's disease. More young tamariki are now developing IBD.
Causes of inflammatory bowel disease
You can't catch IBD from another person. The causes of IBD are unclear but include a range of factors.
Genetic factors (family history)
One in 4 people with Crohn's disease has a relative with Crohn's disease or ulcerative colitis. Recent research into how Crohn's disease runs in families has identified a human gene, called NOD2, which seems to play an important role in the interaction of the body's immune system with gut bacteria.
Ulcerative colitis seems to occur more in some families but it is not clear whether it is due to hereditary or environmental factors.
Immune system
IBD may be a type of autoimmune disease. Some scientists believe the cause of IBD might be a problem in the body's immune system. When your child's immune system tries to fight off infection caused by bacteria or viruses, an unusual immune response causes the immune system to attack the cells in the digestive system
Smoking
It is unknown exactly how smoking is involved with Crohn's disease, but tobacco smoking increases the chance of developing Crohn's disease and makes it more severe.
Diet
There are no specific foods that cause Crohn's disease. There is some evidence that the Western diet may play a role.
Some foods can make symptoms of ulcerative colitis worse for some tamariki but this is very individual.
Signs and symptoms of inflammatory bowel disease
IBD causes parts of the digestive system to become inflamed and ulcerated. The symptoms will depend on which parts and how much of the digestive system is affected.
Symptoms of IBD in children
If your child has IBD (Crohn's or ulcerative colitis), they may have:
- tummy pain
- loose, watery poo (diarrhoea) which may be bloody or have mucus
- bleeding from the bottom (rectal bleeding)
- needing to poo urgently, frequently, and with little warning
- tiredness
- weight loss
- fever
- poor growth
Symptoms of Crohn's disease in children
If your child has Crohn's disease, they may also have:
- loss of appetite
- anaemia or low iron
- nausea
- vomiting
- joint or bone pain
What to do if your child has symptoms of IBD
If you are worried that your child may have IBD, take them to a health professional.
How inflammatory bowel disease is diagnosed
Appointment with a health professional
If you take your child with symptoms of IBD to your health professional, the health professional will ask about your concerns and about your child's health, and examine your child.
Tests
Your child may need some tests that may include:
Blood tests
To look for signs of inflammation, anaemia, nutrient deficiencies.
Poo samples
To look for infection, parasites and inflammation.
Appointment with a paediatrician
Your health professional may arrange an appointment with a paediatrician (specialist children's health doctor).
Endoscopy
If the results of the blood tests and poo samples show that your child is likely to have IBD, then they will need an endoscopy. A doctor uses a flexible tube with a camera attached to the end (an endoscope) and takes small pieces of tissue for testing (biopsies). Your child will usually have a general anaesthetic. During the procedure, the doctor will:
- feed a tube through your child's mouth into their stomach and then the small bowel
- feed another tube from your child's bottom upwards (colonoscopy)
Other tests
If the endoscopy suggests IBD, then your child will need either an MRI or a barium study.
MRI
This is a special type of scan.
Barium study
This is a special type of x-ray called fluroscopy. Your child will drink a special liquid called barium and a technician will take x-rays as the liquid moves through the bowel.
Managing inflammatory bowel disease
Treatment for IBD depends on which parts and how much of the digestive system is affected. It also depends on whether your child has Crohn's disease or ulcerative colitis.
The aims of treatment are to control inflammation, relieve symptoms, make sure your child is growing well and has the vitamins and minerals they need. Some tamariki may need to see a dietitian as part of their treatment.
Sometimes, it's not clear whether a child has Crohn's disease or ulcerative colitis. These tamariki will have a diagnosis of IBDU (IBD unclassified) and receive ulcerative colitis treatment. Whether a child has Crohn's disease or ulcerative colitis may become clear with time.
What is the best diet if my child has inflammatory bowel disease?
If your child has IBD, they can usually eat a normal, balanced diet - anything from any of the food groups.
Ongoing check-ups for your child with inflammatory bowel disease
Tamariki with IBD will have regular check-ups, usually with a paediatrician. It is important to take your child to these appointments and have any blood tests your health professional recommends.
Contact your health professional, paediatrician or gastroenterologist if:
- your child's symptoms are worse or not improving
- your child is losing weight
- the medicines your health professional prescribes are making your child feel unwell
- your child has any new symptoms
How inflammatory bowel disease may affect your child
IBD can be mild and easily controlled in some tamariki and rangatahi (young people). Others may have IBD that is more difficult to manage.
Your child may need to go to the toilet urgently, frequently, and with little warning. The fear of this happening and not being able to get to the toilet in time may cause anxiety, especially for tamariki at school. Talk to your child's school about how best to support them.
Will my child with inflammatory bowel disease be able to lead a normal life?
Yes - with effective treatment, it is possible to manage your child's symptoms and prevent flare-ups. It may take time to work out which treatment is best for your child.
Possible health risks for children with inflammatory bowel disease
People with ulcerative colitis have an increased risk of colorectal cancer. Most people with ulcerative colitis will never develop colorectal cancer. But, because of the increased risk, once people have had ulcerative colitis for 10 years, they will have a colonoscopy every year. The outcome of colorectal cancer in people with ulcerative colitis is excellent because it is picked up early.
People with ulcerative colitis are also at risk of liver disease so liver function monitoring is very important.
When a child has one autoimmune disease, there is a risk of them developing another autoimmune disease such as certain forms of liver disease. Your child will have regular monitoring for this.
More information about support

You can contact Crohn's and Colitis New Zealand for more information and support. They have information for parents, teens and children including a newsletter and support groups.
Camp Purple Live
Crohn's and Colitis New Zealand run a camp - Camp Purple Live. Camp Purple Live also runs a parents' seminar and a junior day. At the parents' seminar, parents can talk to specialist medical professionals to learn more about IBD. At the junior day, kids aged 5 to 9 can experience a day at camp and their parents get some discussion time with a specialist medical professional.
A video all about Camp Purple, run by Crohn's and Colitis New Zealand. Camp Purple is where tamariki and rangatahi can interact with others with similar challenges.
Source: Crohn's and Colitis NZ
Acknowledgements
Illustration by Dr Greta File. Property of KidsHealth.
References
Paediatric Gastroenterology Clinical Network. Management of Inflammatory Bowel Disease in Children and Adolescents in New Zealand. A Clinical Guideline. 2014.
Crohn's and Colitis New Zealand.
The Royal Children's Hospital, Melbourne. Inflammatory bowel disease (IBD) - Crohn disease and ulcerative colitis.
Health Navigator New Zealand. Ulcerative colitis and Crohn's disease.
