Key points about congenital breathing problems
- a congenital problem is one that a baby is born with
- congenital breathing problems can affect how the lungs or airways grow before birth
- scans during pregnancy might show some congenital problems but some are only found after birth
- an operation can help with some problems
- if surgery can’t help, other treatments will focus on keeping your child as well as possible
What is a congenital breathing problem?
A congenital problem is something a baby is born with. It happens while the baby is still developing during pregnancy.
A congenital breathing problem happens when the lungs or parts of the airway don’t grow normally before birth. Some pēpi (babies) may have 1 problem while others may also have problems in other parts of the body.
Scans during pregnancy might show some congenital problems but some are only found after birth.
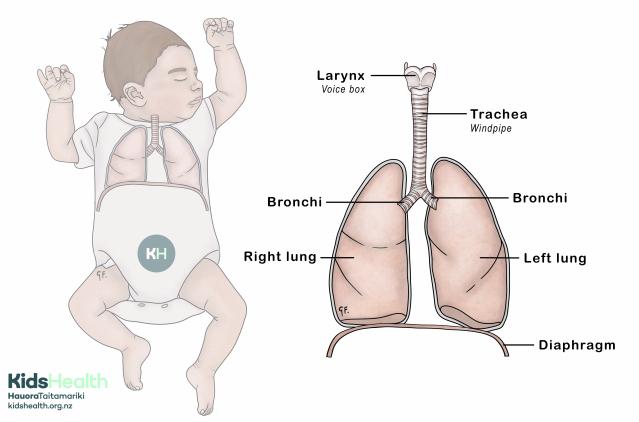
A bit about the lungs and airways
The airways include the mouth and nose, the throat (pharynx), voice box (larynx), windpipe (trachea), bronchi and bronchioles. The airways carry air to the lungs where oxygen can enter the blood.
When we breathe in, air travels down the windpipe (trachea). The trachea splits into the left bronchus and right bronchus.
The diaphragm is a sheet of muscle that sits under the lungs. It separates the chest from the tummy. The diaphragm muscle is important for bringing air into the lungs during normal breathing.
Types of congenital airway problems
There are a few different types of congenital airway problems, and some are more common than others.
-
…
Tracheal stenosis
The trachea is the windpipe. Stenosis means narrowing. Tracheal stenosis is when the windpipe is narrower than it should be. This makes it harder for pēpi and tamariki (children) to move air in and out of the lungs.
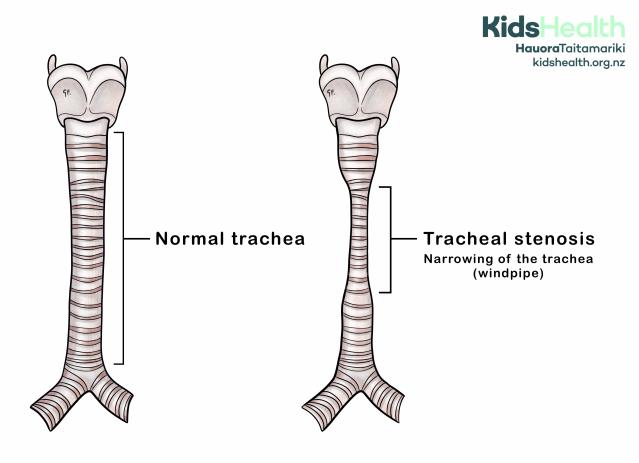
Tracheal stenosis can make pēpi and tamariki more unwell when they have infections like bronchiolitis.
Symptoms of tracheal stenosis can be present even without an infection. They can include:
- noisy or high-pitched breathing (sometimes called wheeze or stridor)
- breathing fast
- working harder to breathe
- getting tired easily, especially with feeding or crying
Tamariki with mild tracheal stenosis may only need regular check-ups and monitoring. Tamariki with more severe tracheal stenosis may need surgery to widen the windpipe.
Tracheomalacia
Tracheomalacia is when the walls of the windpipe (trachea) are soft and floppy, instead of firm. This means the windpipe can collapse slightly when your child breathes in and out. This can make it hard for pēpi and tamariki to move air in and out of the lungs.
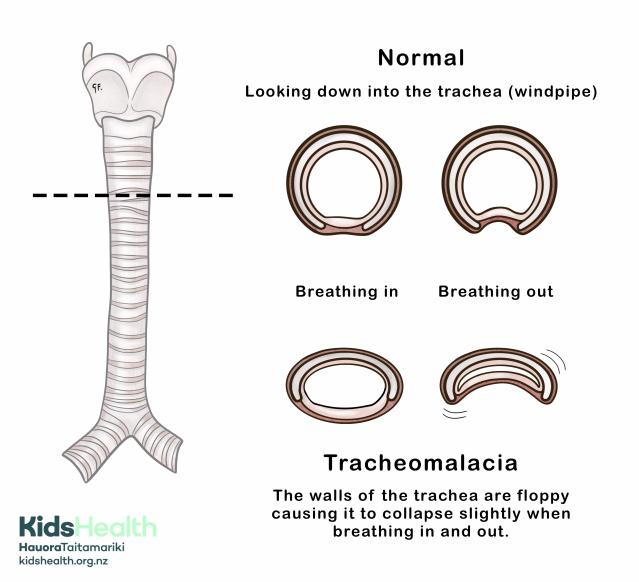
Symptoms of tracheomalacia can include:
- noisy breathing that may improve during sleep
- noisy or high-pitched breathing (sometimes called wheeze or stridor)
- a barking or wet cough even when your child doesn’t have an infection
- trouble breathing, especially when there is an infection
- repeated airway infections
- problems with swallowing
Tamariki with mild tracheomalacia often need no treatment. For many, their symptoms will get better as their airway grows.
Tamariki with more severe tracheomalacia may need chest physiotherapy and even breathing support. Only rarely is surgery helpful.
Tracheo-oesophageal fistula (TOF)
A fistula is an abnormal connection between 2 body parts. A tracheo-oesophageal fistula (TOF) is an abnormal connection between the food pipe (oesophagus) and the windpipe (trachea). This means food or milk can accidentally go into the lungs instead of the stomach.
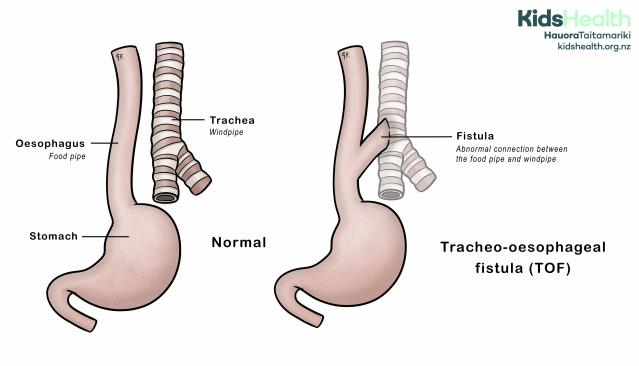
There are different ways that the food pipe and windpipe can connect. The illustration shows just one type.
Symptoms of a TOF are usually seen soon after birth. Symptoms can include:
- coughing or choking when feeding
- frothy bubbles at the mouth
- blue episodes (cyanosis) during feeding
- trouble breathing
- swallowed milk coming back up through the nose
Pēpi with a TOF need surgery to close the abnormal connection between the food pipe and windpipe.
Congenital diaphragmatic hernia
The diaphragm is a big sheet of muscle that sits under the lungs, separating the chest from the tummy. A congenital diaphragmatic hernia is a hole in the diaphragm. Because of this, the intestines or stomach can move from the tummy area into the chest area, squashing the lungs and affecting their growth.
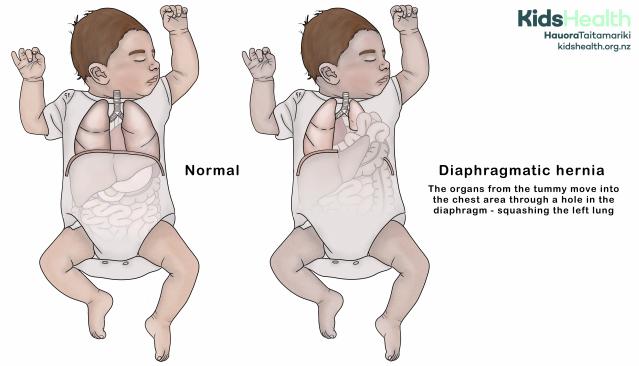
Most pēpi with a diaphragmatic hernia are very unwell when they are born. They can have severe breathing troubles and need treatment immediately.
Pēpi with a diaphragmatic hernia need surgery to close the hole in the diaphragm. There is no medicine to help the squashed lung grow. Rarely, a baby may have such severe damage to their lungs that they may not survive.
Congenital lobar emphysema (CLE)
The lungs are made up of smaller parts called lobes. In congenital lobar emphysema (CLE), 1 lobe of the lung gets over-inflated with air. This can put pressure on other parts of the lung and heart, making breathing difficult.
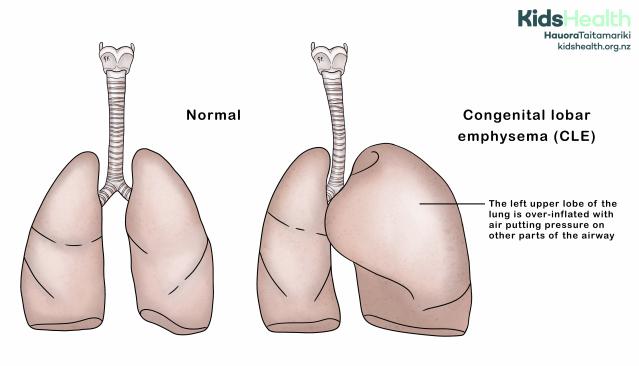
Symptoms of CLE can include:
- breathing problems soon after birth
- a chest that looks uneven or larger on one side
- noisy or fast breathing
Some pēpi with mild CLE may only need monitoring over time. Pēpi with more severe CLE may need surgery. Surgery involves removing the affected lobe to make room for the rest of the lung to grow.
Congenital pulmonary adenomatoid malformation (CPAM)
A congenital pulmonary adenomatoid malformation (CPAM) is where the lung tissue doesn’t form properly. Part of the lung grows as a collection of small or large cysts. This part of the lung tissue doesn’t work properly.
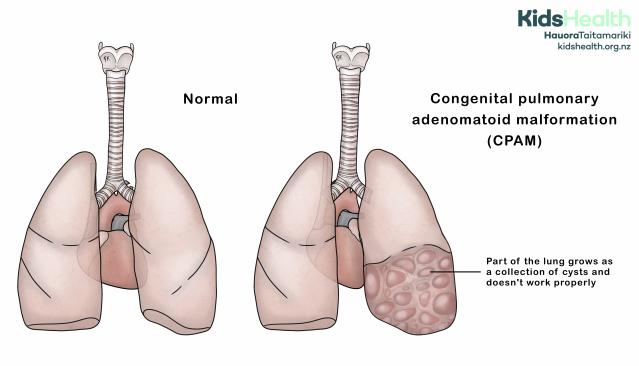
Some tamariki may have breathing difficulties. A child may not have symptoms until they are a teenager, or even an adult.
Treatment can include surgery to remove the part of the lung tissue that is affected.
Can congenital breathing problems be picked up early?
Scans during pregnancy might show some congenital problems, but some are only found after birth. Some of the conditions may not cause symptoms for several months or years after a baby is born.
Treating congenital breathing conditions
Congenital breathing problems that affect the airway can sometimes be treated with surgery. Surgery is not helpful for all conditions that affect the lungs. There are no medicines that can fix the problem. But other treatments can help give the lungs the best chance to grow.
These include:
- oxygen therapy
- tube feeding
- chest physiotherapy
- antibiotics
The best way for a child to get better from a congenital breathing problem is for them to grow as well as possible.
If your child has a congenital breathing problem, your medical team can explain things in more detail.
Acknowledgements
Illustrations by Dr Greta File. Property of KidsHealth.
