Key points about flexible bronchoscopy
- bronchoscopy is a procedure that lets doctors look inside your child's airways
- a bronchoscope is a small camera that also lets doctors take samples of mucus – to test for infection
- bronchoscopy helps doctors diagnose and manage medical conditions
- your child will have a general anaesthetic so they will be fully asleep during the procedure
- if your child is unwell in the first 24 hours after the procedure, and you are worried, take them to your nearest urgent care clinic or emergency department
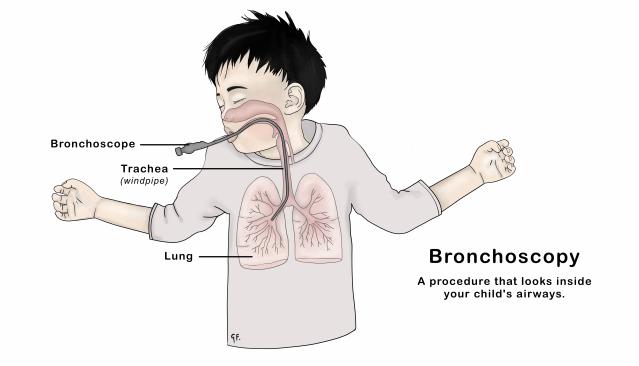
What is a bronchoscopy?
A bronchoscopy is a procedure that shows inside your child's airways. The airways include the voicebox (larynx), windpipe (trachea) and lungs.
A bronchoscope is a small, flexible tube with a camera and light at the end.
A children's respiratory doctor will do the procedure. They specialise in conditions that affect the lungs and are experienced in doing bronchoscopies.
What happens during a bronchoscopy
Looking at the airways
The doctor puts the bronchoscope in through the mouth or nose and then slowly moves it down the windpipe to see into both lungs. The doctor will carefully check the airways.
Your child will be fast asleep from a general anaesthetic. The doctor will also use a spray to numb your child's voice box before putting the bronchoscope down into the airways.
The doctor will take pictures of the lungs and may also record a video of your child's airways using the bronchoscope. These pictures help doctors to diagnose and manage medical conditions. The doctor will put these pictures into your child's medical record.
Taking samples from the airways
Tamariki (children) usually need a "bronchial lavage" during their bronchoscopy. This involves the doctor putting a small amount of salty water (saline) down into the lower airways. The doctor then sucks the fluid back through the bronchoscope into a collection bottle. This fluid contains secretions and mucus from the lungs and airways. The doctor will send this fluid to the laboratory for testing.
CT scan of the airways
Some tamariki also need a CT scan at the same time as the bronchoscopy. CT scans give more information about the lungs than chest x-rays. Your child might need a general anaesthetic if they're having a CT scan. Your child might have both a CT scan and a bronchoscopy under the same general anaesthetic.
See the page on KidsHealth to find out more about CT scans.
Reasons for needing a bronchoscopy
A bronchoscopy helps doctors to diagnose medical conditions. Tamariki may need a bronchoscopy to find a cause for their chest symptoms, including:
- long-lasting cough
- repeated chest infections
- severe wheezing
- unexplained breathing problems
Bronchoscopies help doctors to treat your child's chest problems better. Sometimes, a bronchoscopy shows that there are no problems with the lungs or airways. This is also helpful information and can help doctors to decide how to manage your child's symptoms.
Your child's doctor will explain to you why they think your child needs a bronchoscopy.
Preparation for a bronchoscopy
Sometimes, tamariki need a period of chest physiotherapy or antibiotics before the bronchoscopy. Your child's respiratory doctor will talk to you if this is needed.
What happens during bronchoscopy
Fasting
Your child cannot eat before their procedure. Please check your appointment letter for instructions on when they need to stop eating food.
After stopping all food, your child can only have clear fluids. Clear fluids can be seen through easily. Clear fluids and drinks include:
- water
- lemonade and lemonade ice blocks
- cordial
- clear sports drinks or oral rehydration drinks
Milk and fresh fruit juice are not clear fluids.
General anaesthetic
Your child will have a general anaesthetic and be fast asleep for the whole procedure.
See the KidsHealth page on anaesthesia for more information.
Procedure timing
A bronchoscopy usually takes around 30 minutes. A CT scan also takes about 30 minutes. Ask your doctor on the day how long the whole process might take.
Recovery
After the bronchoscopy, your child will go to a recovery area. You can join them there.
The respiratory doctor will talk to you after the bronchoscopy to discuss the findings and show you the pictures that were taken. Usually, the doctor will give parents a copy of the report that goes into your child's medical record.
Going home after a bronchoscopy
Tamariki can usually go home the same day, around 3 to 5 hours after the bronchoscopy. Some tamariki may need to stay overnight in a hospital ward so doctors can monitor them.
Your child will need to spend the night in hospital if they:
- are less than 12 months old or
- have complicated health problems
- need to have oxygen overnight after the bronchoscopy
- need further treatment
- have had another operation on the same day (for example, having their tonsils removed)
Your child's respiratory doctor will tell you if you should come prepared for your child to stay overnight.
If you have to travel to another centre for your child's bronchoscopy, your child's doctor may recommend you stay locally overnight after the procedure. Your local hospital will help arrange accommodation.
What to expect after a bronchoscopy
General anaesthetic
Your child should be able to return to normal activities, including school, the day after the anaesthetic.
Rangatahi (young people) should not operate machinery, drive or make important decisions for the rest of the day after their procedure.
Diet
The doctor used a spray to numb your child's voice box before the bronchoscopy. Your child cannot eat or drink until this has worn off. It usually takes about 3 hours.
Possible side effects from a bronchoscopy
Usually, tamariki manage very well with bronchoscopies.
After a bronchoscopy, it is common for tamariki to:
- have a hoarse voice
- have a sore throat
- cough more
- have a fever
You can give your child paracetamol if they have a fever after their bronchoscopy. You must follow the dosage instructions on the bottle. It is dangerous to give more than the recommended dose.
If your child has had bronchial lavage, there's a very small chance they could cough up blood-stained fluid. This is likely to look like very weak blackcurrant juice.
Rarely, some tamariki may need oxygen for a few hours after the procedure. Very rarely, tamariki might need to go to the intensive care unit for help with their breathing after a general anaesthetic. If your child is at risk for this, your doctor will discuss this with you before the bronchoscopy.
Bronchoscopy results
Lab samples
Your child's respiratory doctor will speak to you after the procedure to let you know how it went. If the doctor sends any samples to the lab, it can take a week or two to get the results.
CT scan
If your child had a CT scan, you will get these results once the radiologist has looked at the scan images and written a report. This can also take a week or two.
Bronchoscopy
The doctor who did the bronchoscopy will send your child's doctor a report of everything. You will get a copy of the same letter. The letter will include:
- the findings of the bronchoscopy
- results from any samples and scans
- any changes to treatment
- if any further tests are needed
The doctor will make a plan with you on how to follow up on these results. They may ask you to contact your child's local paediatrician if you haven't received any results after a few weeks.
When to get medical help after a bronchoscopy
In the 24 hours after the bronchoscopy, if your child has any of the following symptoms, take them to the nearest emergency department.
Important symptoms include:
- difficulty breathing
- a cough that is getting worse
- coughing up fresh blood
- chest pain
- fever (temperature over 38 degrees Celsius) that doesn't get better after giving paracetamol
- being worried in any way about your child
Acknowledgements
Illustration by Dr Greta File. Property of KidsHealth.
