Warfarin management guide for rheumatic heart disease
The information on this page is from the booklet Warfarin Management Guide for Rheumatic Heart Disease by Te Whatu Ora | Health New Zealand.
Share or print a PDF version of the booklet in your preferred language.
Why do you need warfarin?
You have had a new valve (or two) put in your heart to replace the one(s) damaged by rheumatic fever. Your new mechanical heart valve helps your heart work better. That's great news. But, the new valve(s) makes it more likely your blood will form a clot.
Blood clots can travel from your heart to other parts of your body through your blood vessels.
If this happens, it can stop the flow of blood to important places like your brain or heart. Blood carries oxygen to these organs. If the blood supply is cut off by a clot, the cells that make up these organs can die. This leads to a stroke or a heart attack. This could make you extremely sick and could leave you disabled, or you could die.
Warfarin brands
In Aotearoa New Zealand, warfarin comes in 2 different brands of tablets. The 2 brands are not exactly the same - it's important to keep taking the same brand.
Marevan® is the brand of warfarin that is usually used in New Zealand.
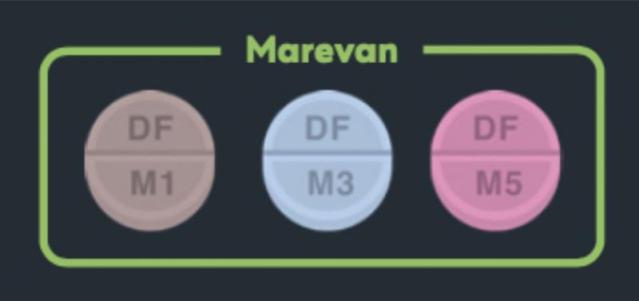
Coumadin® is another brand of warfarin. It cannot be used at the same time as Marevan®.

Warfarin tablets come in different strengths. It's important to only take the warfarin that has been prescribed for you.
How to take warfarin
Warfarin helps prevent blood clots forming in your body. Your doctor, pharmacist or other health professional will tell you how much warfarin you need to take. It's important to follow these instructions.
See the KidsHealth page about how to take warfarin for rheumatic heart disease.
Taking Warfarin For Rheumatic Heart Disease
Daily dosage
Make sure to take your warfarin tablet every day.
Your health professional may advise you to take your warfarin in the evening. This is because you usually have your blood tests (to monitor INR) in the morning.
You may prefer to take your warfarin at dinner time. You can take it before, during or after your meal.
Use a calendar or reminder system on your phone to mark off when you have taken your daily dose
Early or late doses
If you forget to take your warfarin tablet at your normal time, this is fine. You can still take your warfarin tablet for that particular day.
For example, if you normally take your warfarin at 6pm every day but at 9pm you realise that you have forgotten to take your warfarin - you can still safely take your warfarin.
Same applies if you have taken your warfarin early. A few hours before or after will not cause any harm.
Missed dose
If you have completely forgotten to take your warfarin tablet for the day, and only realised the next day, take your normal warfarin dose and contact your health professional immediately.
DO NOT DOUBLE DOSE. Do not take 2 warfarin tablets in one day. This will have the opposite effect and can be harmful. Your health professional will advise you what to do.
If you miss 2 or more doses, tell your health professional as soon as you can.
Monitoring and blood tests
Your health professional needs a reliable way to monitor what's going on in your blood so they can prescribe a safe warfarin dose for you. So you will need regular blood tests to measure your INR.
INR testing
You need regular blood tests to measure your INR (international normalized ratio). Your INR shows how long your blood takes to clot. Your health professional will tell you what INR number is right for you. If you're unsure, ask the health professional managing your warfarin.
Ways to monitor your INR
There are a number of ways to monitor your INR - such as at home or at the pharmacy. It's important you understand how this is going to happen for you. If you are unclear, ask your health professional to explain this to you.
Monitoring at home
Some people prefer to check their blood at home rather than going to a laboratory. At home monitoring involves finger prick testing with a portable machine. You have to pay for the INR test strips.
Monitoring at the pharmacy
Once your INR is stable, you may be able to go to a pharmacy for INR monitoring using finger prick testing. Your health professional can give you more information about this.
How often to monitor your INR
In the beginning, you will need daily blood tests until your INR is stable. This is usually for 1 to 2 weeks. Later, you may need blood tests every 2 to 4 weeks or as often as your health professional advises you.
Adjusting the warfarin dose
Your health professional will tell you what dose of warfarin to take based on your INR results. Your INR may take 2 to 4 days to change following a change to your warfarin dose.

Warfarin side effects
The main side effects to watch out for are increased bleeding and bruising. This happens because warfarin slows down the blood’s clotting system. When your INR is at the correct level, the risk of side effects is low.
Bleeding
Warfarin can cause more bleeding and bruising than normal. See a health professional immediately, or go to an emergency department, if:
- you have a serious fall or hit to the head
- you have any serious symptoms like coughing up blood or vomiting blood
- there is blood in your urine or bowel motions
- you have bleeding that won't stop after 10 minutes of applying pressure
For women, if you notice heavier bleeding during your period than before starting warfarin, continue your warfarin and see a health professional. There are ways to manage heavy periods.
Other side effects
Very occasionally warfarin can cause:
- vomiting
- nausea
- diarrhoea
- rash
- hair loss (alopecia)
If you experience any of these things talk to your health professional.
Things to watch out for
Early signs that your warfarin dose may need changing
Watch for early signs of bleeding such as:
- unexpected bruises
- bleeding gums
- nosebleeds
Let your health professional know if you have any of these.
Injuries
Avoid activities that might cause injuries and see a health professional urgently if you have any signs of serious bleeding, such as:
- coughing or vomiting blood
- nose bleeds that don't stop after a few minutes
- blood in urine or bowel motions
- severe headache
- dizziness or weakness
Monthly Bicillin IM injections
The nurse giving your IM (intramuscular) injection should check your latest INR result before giving your antibiotic. In most cases, it will be safe to give your IM injection but there is a chance you may get a bruise following this.
When to see a health professional urgently
If your INR is too low it might not be preventing clots so go to the nearest emergency department immediately if you have:
- difficulty breathing
- pain in your chest
- pain
- swelling in your legs
Go to the nearest emergency department immediately if you have any symptoms of a stroke such as:
- face drooping
- arm weakness
- speech difficulty
- confusion
- trouble seeing
- trouble walking
Whānau should also be aware of symptoms of a stroke so they can get help immediately.

Diet and lifestyle
You need regular blood tests because many things can affect your INR. This includes:
- what you eat
- other medicines
- vitamins and supplements
- illness
To keep your INR stable, try to eat a balanced diet. Let your health professional know of any lifestyle changes (such as loss of weight, eating more healthily, or starting to take vitamins or supplements). These can affect your INR.
Vitamin K
Vitamin K can lower the effect of warfarin.
Some foods have a lot of Vitamin K in them such as:
- broccoli
- spinach
- watercress
- silver beet
- green leafy vegetables
- brussel sprouts
- dark green lettuce
- turnip greens
- chickpeas
- soybeans
- liver
It's best to keep eating the same amount of these each day to keep your INR stable.
Other foods can increase the effect of warfarin, such as garlic.
Alcohol
Too much alcohol can mean you have a higher chance of severe bleeding even while your INR is still in the target range. Don't drink more than 1 to 2 standard alcohol drinks in one day. One standard drink is 300ml regular beer or 100ml wine or 30ml spirits (whisky, gin, vodka).
Herbal drinks and supplements
Other drinks and herbal supplements to avoid if you are taking warfarin include:
- herbal teas such as chamomile or kawakawa
- herbal drinks such as kava, noni juice or cranberry juice
- herbal supplements such as ginko biloba, garlic, ginseng, St. John’s Wort, ginger, fenugreek, papaya, dong quai, red clover, feverfew, echinacea purpurea
- any supplements containing vitamin K
- any products with sources of vitamin K (alfalfa tablets, Anlene® dairy products)
- dietary supplements which have large amounts of Vitamin E and Omega 3 fatty acids, Co-Enzyme Q10
Other medicines
Tell your health professionals about all other medicines, supplements, or herbal remedies you take. These can affect warfarin. Remind them you are on warfarin if you need new medicines.
When taking warfarin, don't take anti-inflammatory medicines like ibuprofen (Brufen, Nurofen) and diclofenac (Voltaren).
Travel and daily activities
While you are on warfarin, take extra care to avoid doing things that could cause bruising or bleeding such as deep massage.
Travel
You can travel with warfarin. But let your health professional know your travel plans if you are going to be away when your INR blood test is due. You may need a blood test before you leave or while you're away.
Carry your warfarin in your carry-on luggage. Your health professional can give you a letter saying that you are travelling with essential medicines for your own use.
Moving permanently
Tell your health professional and your heart specialist if you are planning to move away permanently, or for longer than 3 months. They can help by referring you to the medical team in your new area. They can give you a letter and a copy of your medical records to take with you.
Physical activity
Avoid contact sports (like rugby or boxing). Avoid activities with a high risk of falling or bumpy rides such as theme park rides. If you're not sure, check with your health professional.
Tattooing
There is a risk of bruising and bleeding with tattooing. Generally, it's not recommended but talk to a health professional for advice.
If you are going to have a traditional tattoo, talk to your health professional. They will need to manage your warfarin around the tattooing.
Very important things to remember
Pregnancy
If you are considering pregnancy, your health professional can arrange for you to talk with a specialist or heart doctor who looks after people with heart disease in pregnancy. This can happen at any time, even if you are not planning a pregnancy immediately.
To avoid an unplanned pregnancy, use some form of contraception until you are ready for pregnancy. Talk with your health professional about what is best for you.
If planning a pregnancy, you may need to change your medicines before you become pregnant. Warfarin can harm a baby's development in early pregnancy. There are other medicines which will reduce the chance of clots and are safer for baby.
If you find out you are pregnant, please talk to your health professional as soon as you can so that they can change your medicines if needed. Don't just stop taking your warfarin. Your health professional will discuss the best options for blood thinners with a specialist obstetrician (a doctor who looks after pregnant people) and your heart specialist.
Keep your health professionals up to date
Let your health professionals know if you have missed or taken extra doses of warfarin, if you have made any changes to what you eat or other lifestyle changes.
Also, let your health professional know if you are taking any herbal remedies, kawakawa tea, or vitamin supplements. medicines, and painkillers.
Be honest with your health professional. For example, if you've missed some doses and your INR is low, tell your health profesional. If they don't know you've missed some doses, they may increase your warfarin dose. This leads to a high INR and an increased risk of bleeding.
Tell your dentist
Tell your dentist you are taking warfarin. Consider using a soft toothbrush if your gums bleed easily.
Medical procedures
If you need to have even small medical procedures, always let the health professional know that you are on warfarin.
Emergencies
Consider getting a MedicAlert bracelet or necklace in case you are unable to tell someone that you are taking warfarin (such as a car accident).
Overdose
If you ever suspect that you or someone else has swallowed too many warfarin tablets, call your National Poisons Centre for advice. In Aotearoa New Zealand, that's 0800 POISON or 0800 764 766.
By following these guidelines and regularly talking to your health professional, you can manage your warfarin therapy effectively and reduce the risk of complications.
Warfarin book
Keep your warfarin record updated and bring it to all medical appointments.
